Orthognathic surgery, also known as corrective jaw surgery is the use of surgical procedures to correct imbalance in the upper and lower jaws. These procedures may be used to treat an abnormality where the teeth do not fit together properly (malocclusion), to treat airway obstruction when a patient is asleep (obstructive sleep apnea), or to improve the balance and overall appearance of the face. Often patients who are undergoing orthodontic treatment with braces may find that an imbalance of their jaws make it impossible for their bite to be corrected without repositioning the jaws. Treatment with orthognathic surgery is carried out with combined management between an orthodontist and a maxillofacial surgeon.
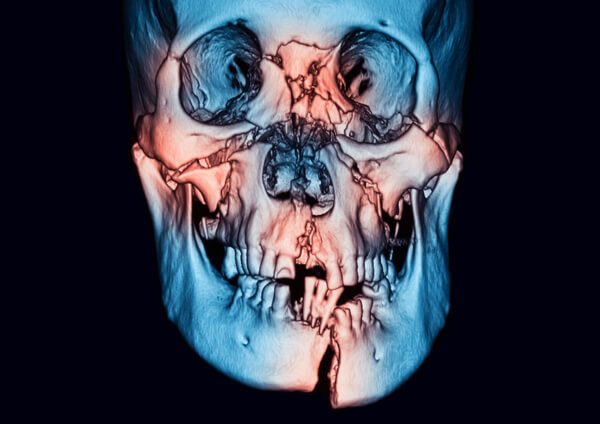
There are many other bones that are found deeper within the facial structure. Muscles required for chewing, swallowing and talking are attached to these bones.
Nasal fractures (broken nose) are the most common. Fractures to other facial bones can also occur. You might only have one fracture, or you might have several broken bones. Multiple fractures are more likely to occur during a motor vehicle accident or other high-impact accident. Fractures may be unilateral (occurring on one side of the face) or bilateral (occurring on both sides of the face).
If you suffer from a facial injury, you should seek immediate medical attention. Some fractures are minor. However, complex fractures may cause irreversible damage and can even be life-threatening.
Located near to the bones in your face are the nerves and muscles that are responsible for sensations, expressions and eye movements. The muscles and nerves are located near to the facial bones. The face is close to the brain and central nervous system (CNS). Fractures may result in damage to cranial nerves, depending on the particular type and location of the fracture. Fractures to the orbit (eye socket) may result in problems with vision. Fractures of the nose may make it difficult for the injured person to breathe or smell. Also, fractures of the jawbones may cause breathing problems or make it difficult to chew, speak, or swallow.
There are several main types of facial fractures.
Nasal bones (broken nose): Nasal bone fractures are the most common type of facial fracture. The nasal bone is made up of two thin bones. It takes less force to break the nasal bones than other facial bones because they are thin and prominent. Usually, the nose looks deformed or feels sore to the touch after a fracture. Swelling in the area might make it more difficult to assess how much damage has occurred. Nosebleeds and bruising around the nose are common symptoms of a nasal fracture.
Symptoms of a nose fracture may include:
Mid-face (Le Fort fractures): Blunt force trauma tends to cause fractures along three lines of weakness in the mid-face. One characteristic of all types of Le Fort fractures is the fracture of the pterygoid processes, part of the sphenoid bone. There are three main types of Le Fort fractures, but there may be individual variations.
Mandible (lower jaw): The mandible holds the lower teeth in place and moves when you are talking or chewing. Fractures of the lower jaw affect the sections of the lower jaw that supports teeth (called the body), the part where the jaw curves upwards into the neck (the angle) or the knob-shaped joint at the top of the jaw bone (the condyle) or the point where the two sides of the lower jaw are joined (the symphysis). If you have a break in the lower jaw, you may also have broken or loose teeth.
How are facial fractures treated?
Your healthcare provider may prescribe pain-relieving drugs as well as oral steroids to ease swelling. Your provider will prescribe antibiotics if there’s a high risk of infection.
In general, fractures may be treated by performing a closed reduction (resetting the broken bone or bones without surgery) or an open reduction (surgery that requires an incision to reposition the fractured bones). For a complex fracture with multiple broken bones, you will need reconstructive surgery.
The type of treatment will depend on the location and extent of the injury. The aim of treatment for facial fractures is to restore the normal appearance and function of the injured areas.

The results from the procedure are permanent. Once you remove those fat pads, they are gone for good. Although your buccal fat pads won’t grow back, weight gain can mask the results of the procedure. As you age, you may see fat start to descend into the lower part of the face as well.
Your face will likely look fuller during your recovery. But after the swelling goes down, you should start to see the final result. Swelling should subside in approximately 3 weeks. It can take as long as 3 to 6 months to see the final result. During this time, your skin is settling into its new position after the fat is hollowed out.
Over a period of time, the jawbone associated with missing teeth atrophies (shrinks) or recedes. This often results in the presence of less than adequate bone density/volume suitable for placement of dental implants. In the past, most patients in this situation were denied the placement of dental implants.
Today, we have the techniques and biomaterials to graft or grow bone where needed. This not only gives us the opportunity to place implants of sufficient sizes in the prosthodontics guided 3D position, it also gives us a chance to restore functionality and aesthetic appearance.
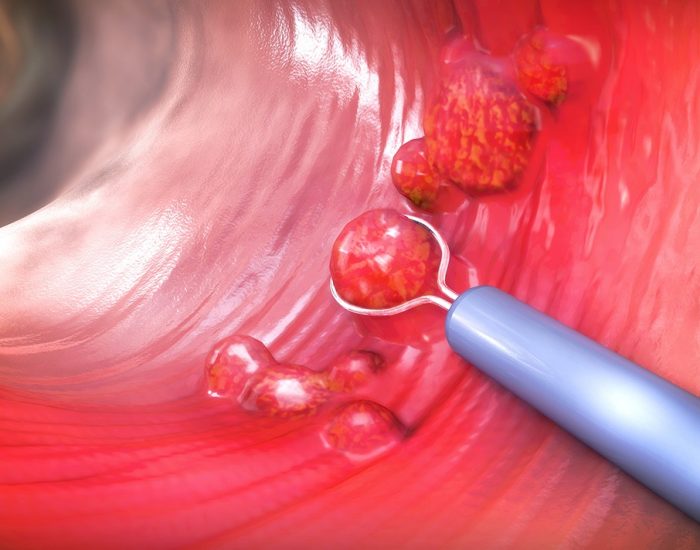
Minor bone grafting such as immediate socket augmentation after an extraction, can repair potential implant sites with damaged bone structure due to previous extractions, infections, gum disease or injuries.
There are different Biomaterials that are commonly used for minor augmentations with “bone in a bottle”. These have animal, human or purely synthetic origin and include: a) bone elements of cow bone origin (xenograft), b) bone from human donor origin obtained by tissue banks as part of multi-organ donor scheme, c) synthetic bone of calcium phosphate origin or d) your own bone is taken from the jaw, hip or tibia (below the knee). For minor augmentations normally xenografts of cow bone origin are used with long term safety and efficacy shown through extensive clinical studies spanning over decades both in orthopaedic surgery and oral surgery.
We use your own growth factors obtained from a sample of your own blood to accelerate and promote bone and soft tissue formation in graft areas. This regenerative medicine technique is known as Platelet Rich Plasma (PRP) or Platelet Rich Fibrin (PRF).
No, socket preservation bone grafts aren’t necessarily required every time a tooth is extracted, – this depends on the patient’s age, biotype, the location of the extracted tooth, and the overall oral health of the patient. In some cases, extraction sites can heal completely fine on their own, resulting in sufficient bony ridge height and horizontal ridge width for implant placement.
However, with complicated extractions, a lot of alveolar bone can be lost, and adding a bone graft at the time of removal can prevent the socket walls from caving in, providing a solid, firm foundation for the future dental implant.
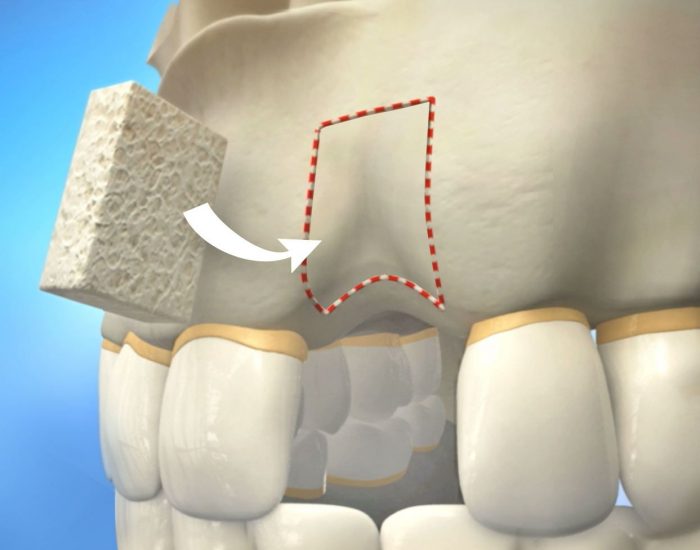
Sinus lift bone grafts are indicated commonly to replace bone in the back of the upper jaw when replacing back teeth (molars).
The Maxillary sinus is a medium size empty air cavity located within the upper jaw bone where the roots of molar teeth are normally embedded. When these upper teeth are removed, there can be a thin layer of bone left to separate the maxillary sinus from the mouth. When the sinus wall is very thin, it may not be possible to place traditional dental implants in this area. The procedure to augment or grow bone below the floor of the maxillary sinus cavity is called a “sinus lift graft” or “sinus augmentation”.
To place implants, the floor of this air cavity bordering the teeth is filled with bone substitutes or biomaterials. A xenograft (cow bone origin) is the material of choice for this procedure used very safely and successfully over decades. Special dissolving membranes are used under the gum to protect the bone graft and encourage bone regeneration. This is called guided bone regeneration (GBR). Membranes can be synthetic or porcine in origin.
If there is a borderline amount of bone remaining between the ridge of the upper jaw and the floor of the sinus cavity to stabilize the implant, sinus augmentations and dental implant placement can sometimes be performed as a single procedure. This is known as “simultaneous sinus lift” meaning that it is carried out at the time of implant placement. If not enough bone is available, the sinus lift is performed first and the graft is allowed to mature for a few months ( 6 to 8 months). Once the graft has matured, the implants can be placed. This is referred to as “staged sinus lift”.